In 2000 the German Brain Tumour Association developed World Brain Tumour Day.
The goal is to direct international public attention to people that are confronted with this serious disease and the urgent need for more research. Every year on this day there are a wide variety of events taking place around the world.
Contd…
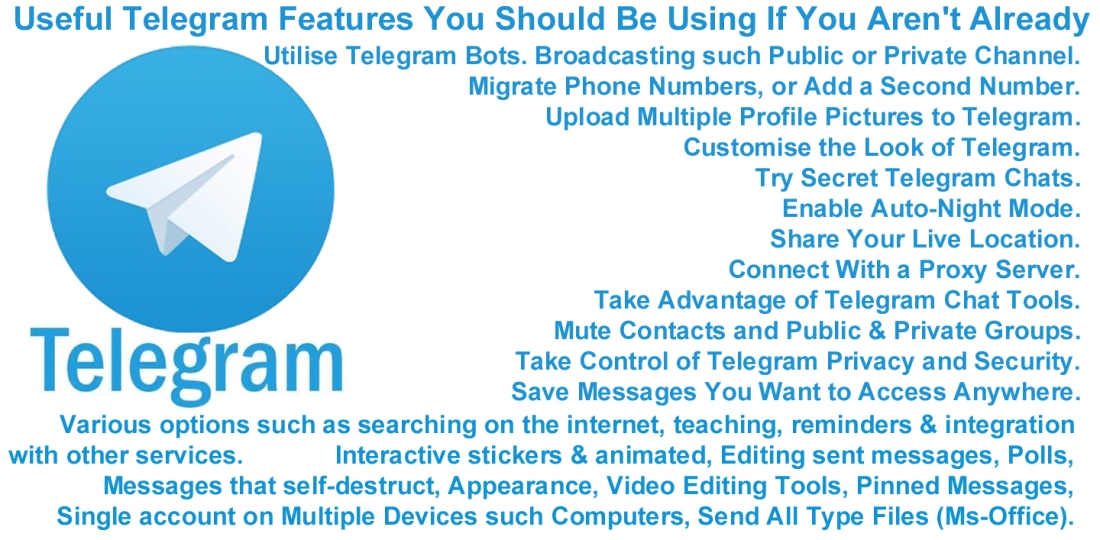
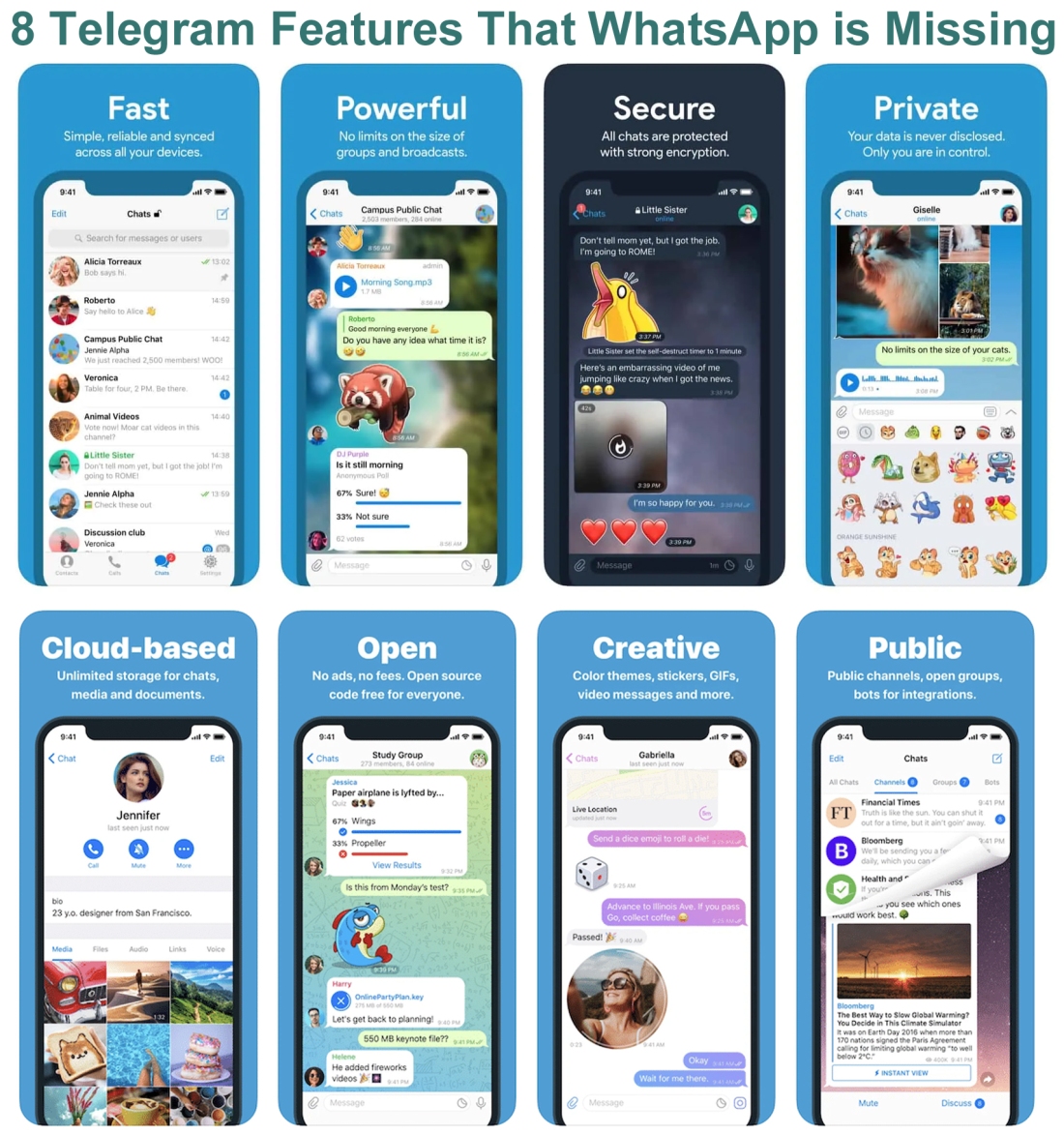
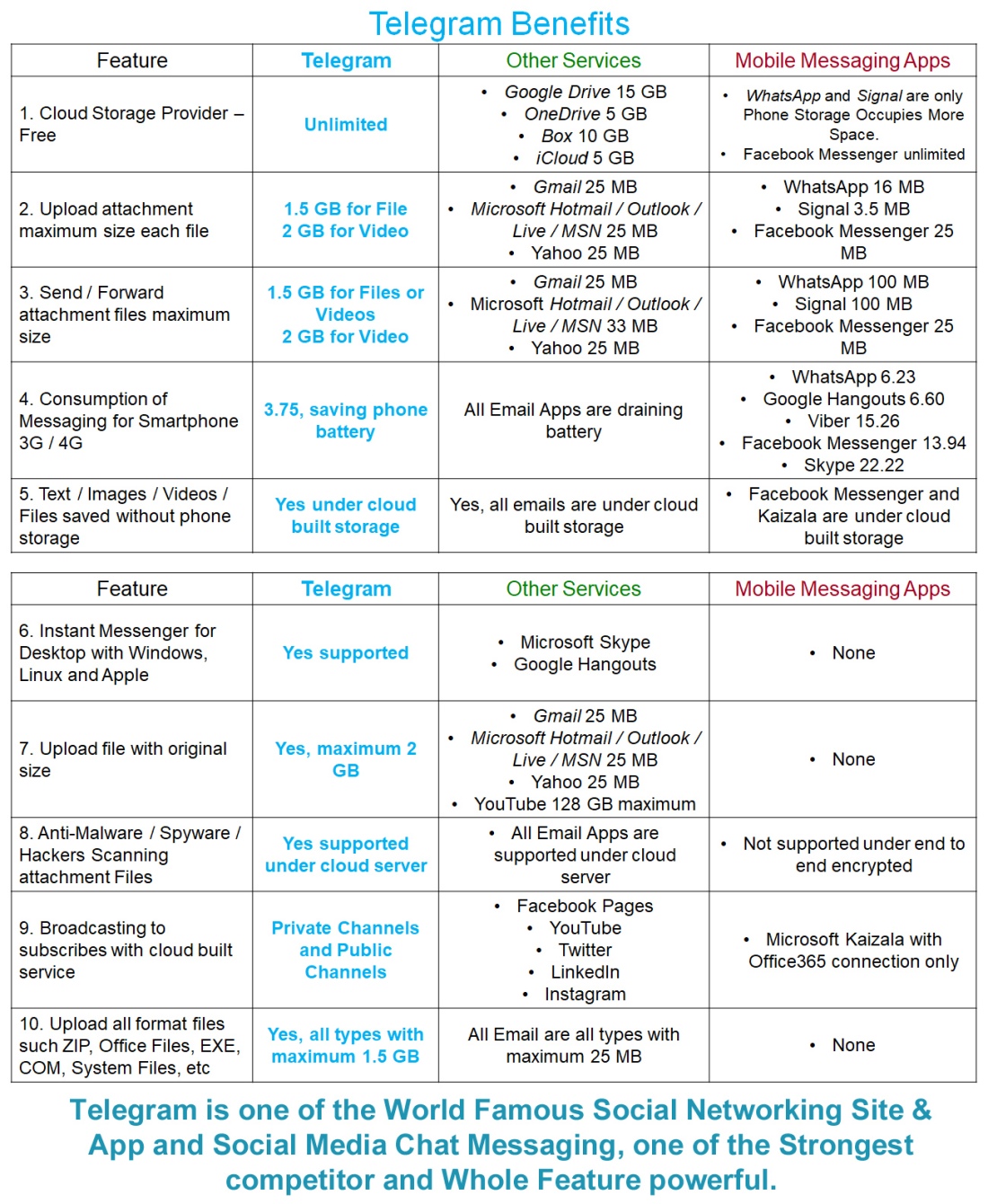
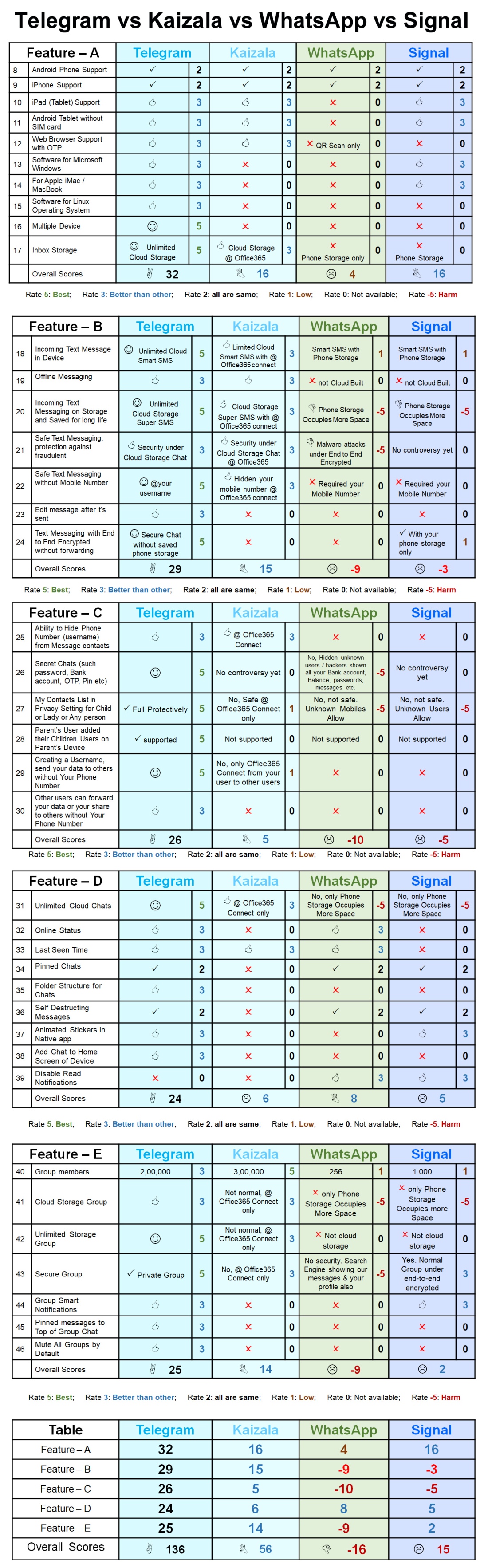
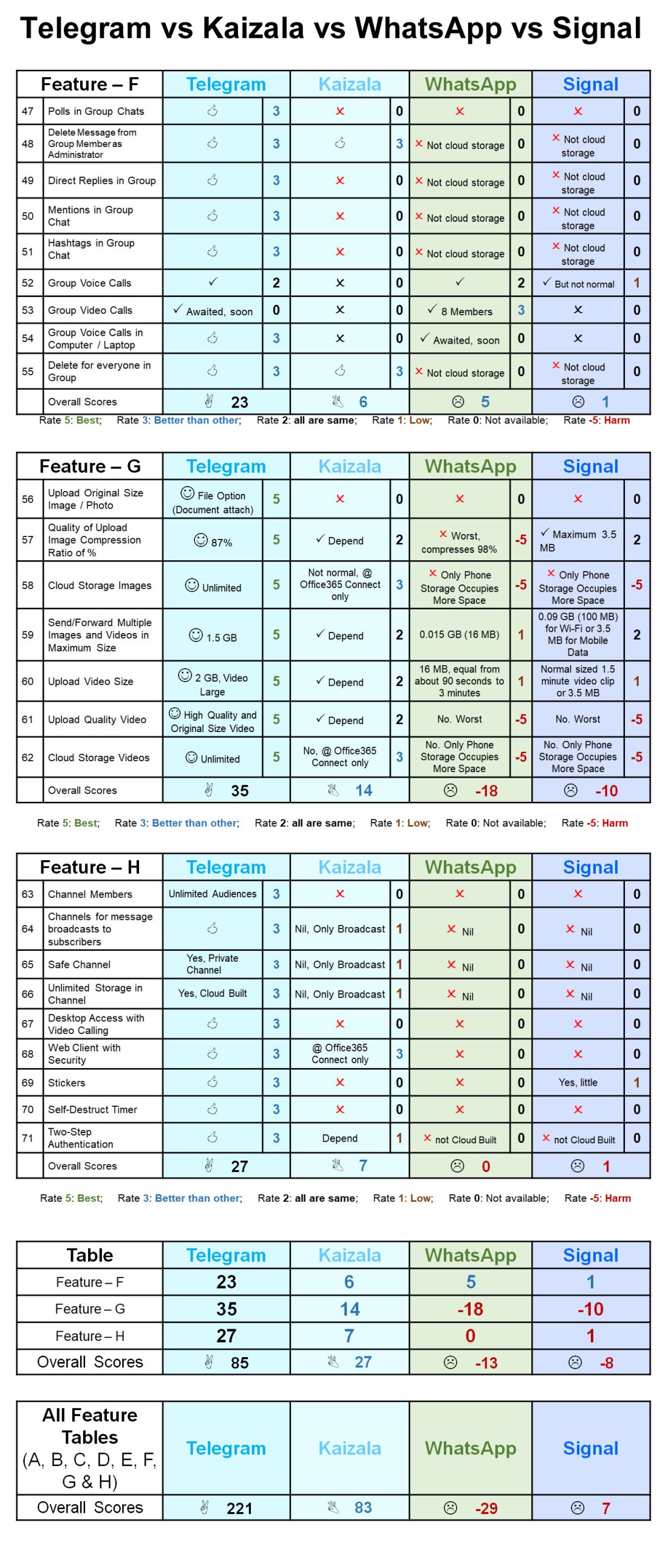
Telegram provides unlimited server storage. This means all your text messages, images media files & documents will be saved on their cloud without losing any data, you don’t need to worry about backup & restore. Telegram Private Groups cannot be found with an in-app search. The group is private, after all that you can use the 2,00,000 member limit fully. Telegram Channels are a tool for broadcasting public (or) private messages to large audiences, similarly as you do on Twitter or Facebook Page. In fact, channels can have an unlimited number of subscribers. Telegram Private Channels cannot be found with an in-app search. Group video calls on Telegram allow 30 users to broadcast from their camera as well as their screens. This can now be watched by 1,000 people at once (updated by 1st August 2021). Users can hold anything event online, from lectures to concerts and everything in between, similarly as Zoom or Microsoft Teams or Google Meet.
Join Us
| Telegram Channel | Twitter | LinkedIn Page | Microsoft Teams | Other Social | WhatsApp Channel | Blogger |
A brain tumour occurs when abnormal cells form within the brain. There are two main types of tumours: cancerous (malignant) tumours and benign tumours. Cancerous tumours can be divided into primary tumours, which start within the brain, and secondary tumours, which have spread from elsewhere, known as brain metastasis tumours. All types of brain tumours may produce symptoms that vary depending on the part of the brain involved. These symptoms may include headaches, seizures, problems with vision, vomiting and mental changes. The headache is classically worse in the morning and goes away with vomiting. Other symptoms may include difficulty walking, speaking or with sensations. As the disease progresses, unconsciousness may occur.
The cause of most brain tumours is unknown. Uncommon risk factors include inherited neurofibromatosis, exposure to vinyl chloride, Epstein–Barr virus and ionising radiation. Studies on mobile phone exposure have not shown a clear risk. The most common types of primary tumours in adults are meningiomas(usually benign) and astrocytomas such as glioblastomas. In children, the most common type is a malignant medulloblastoma. Diagnosis is usually by medical examination along with computed tomography (CT) or magnetic resonance imaging (MRI). The result is then often confirmed by a biopsy. Based on the findings, the tumours are divided into different grades of severity.
Treatment may include some combination of surgery, radiation therapy and chemotherapy. Anticonvulsant medication may be needed if seizures occur. Dexamethasone and furosemide may be used to decrease swelling around the tumour. Some tumours grow gradually, requiring only monitoring and possibly needing no further intervention. Treatments that use a person’s immune system are being studied. Outcome varies considerably depending on the type of tumour and how far it has spread at diagnosis. Glioblastomas usually have very poor outcomes, while meningiomas usually have good outcomes. The average five-year survival rate for all brain cancers in the United States is 33%.
Contd…

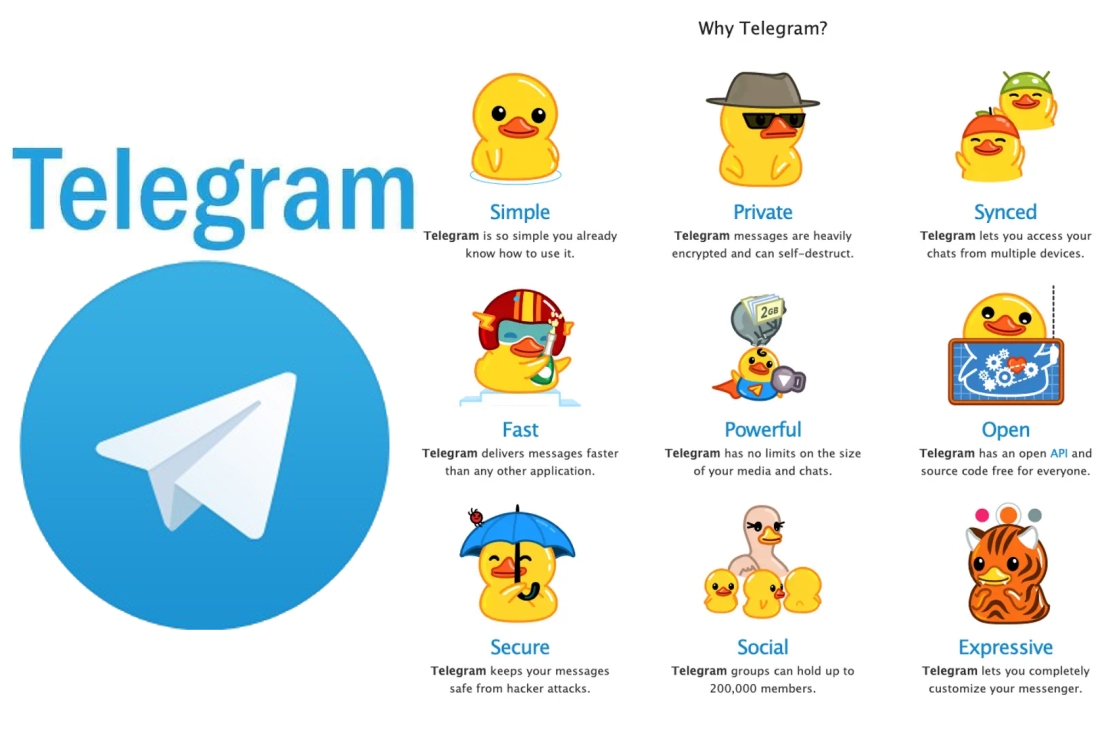
A. Simple: Telegram is so simple you already know how to use it.
B. Private: Telegram messages are heavily encrypted and can self-destruct.
C. Synced: Telegram lets you access your chats from multiple devices.
D. Fast: Telegram delivers messages faster than any other application such WhatsApp, Signal etc.
E. Powerful: Telegram has no limits on the size of your media and chats.
F. Open: Telegram has an open API and source code free for everyone.
G. Secure: Telegram keeps your messages safe from hacker attacks.
H. Expressive: Telegram lets you completely customise your messenger.
Join Us
| Telegram Channel | Twitter | LinkedIn Page | Microsoft Teams | Other Social | WhatsApp Channel | Blogger |
Secondary, or metastatic, brain tumours are about four times more common than primary brain tumours, with about half of metastases coming from lung cancer. Primary brain tumours occur in around 250,000 people a year globally, making up less than 2% of cancers. In children younger than 15, brain tumours are second only to acute lymphoblastic leukemia as the most common form of cancer. In Australia, the average lifetime economic cost of a case of brain cancer is $1.9 million, the greatest of any type of cancer.
Signs and symptoms
The signs and symptoms of brain tumours are broad. People with brain tumours will experience them regardless of whether the tumour is benign (not cancerous) or cancerous. Primary and secondary brain tumours present with similar symptoms, depending on the location, size, and rate of growth of the tumour. For example, larger tumours in the frontal lobe can cause changes in the ability to think. However, a smaller tumour in an area such as Wernicke’s area (small area responsible for language comprehension) can result in a greater loss of function.
Headaches
Headaches as a result of raised intracranial pressure can be an early symptom of brain cancer. However, isolated headache without other symptoms is rare, and other symptoms often occur before headaches become common. Certain warning signs for headache exist which make it more likely to be associated with brain cancer. These are as defined by the American Academy of Neurology: “abnormal neurological examination, headache worsened by Valsalva maneuver, headache causing awakening from sleep, new headache in the older population, progressively worsening headache, atypical headache features, or patients who do not fulfill the strict definition of migraine”.
Location specific symptoms
The brain is divided into 4 lobes and each lobe or area has its own function. A tumour in any of these lobes may affect the area’s performance. The location of the tumour is often linked to the symptoms experienced but each person may experience something different.
- Frontal lobe tumours may contribute to poor reasoning, inappropriate social behavior, personality changes, poor planning, lower inhibition, and decreased production of speech (Broca’s area).
- Temporal lobe: Tumours in this lobe may contribute to poor memory, loss of hearing, difficulty in language comprehension (Wernicke’s area).
- Parietal lobe: Tumours here may result in poor interpretation of languages and difficulty speaking, difficulty writing, drawing, naming, and recognising, and poor spatial and visual perception.
- Occipital lobe: Damage to this lobe may result in poor or loss of vision.
- Cerebellum: Tumours in this area may cause poor balance, muscle movement, and posture.
- Brain stem: Tumours on this can cause seizures, induce endocrine problems, respiratory changes, visual changes, headaches and partial paralysis.
Behavior changes
Despite the personality and behavior changes that occur in people with brain tumours, little research on such changes has been done. A person’s personality may be altered due to the tumour damaging lobes of the brain. Since the frontal, temporal, and parietal lobes control inhibition, emotions, mood, judgement, reasoning, and behavior, a tumour in that region can cause inappropriate social behavior, temper tantrums, laughing at things which merit no laughter, and even psychological symptoms such as depression and anxiety.
Personality changes can have damaging effects such as unemployment, unstable relationships, and a lack of control.
Cause
Epidemiological studies are required to determine risk factors. Aside from exposure to vinyl chloride or ionising radiation, there are no known environmental factors associated with brain tumours. Mutations and deletions of tumour suppressor genes, such as P53, are thought to be the cause of some forms of brain tumour. Inherited conditions, such as Von Hippel–Lindau disease, multiple endocrine neoplasia, and neurofibromatosis type 2 carry a high risk for the development of brain tumours. People with celiac disease have a slightly increased risk of developing brain tumours.
Although studies have not shown any link between cell phone or mobile phone radiation and the occurrence of brain tumours, the World Health Organisation has classified mobile phone radiation on the IARC scale into Group 2B – possibly carcinogenic. Discounting claims that current cell phone usage may cause brain cancer, modern, third-generation (3G) phones emit, on average, about 1% of the energy emitted by the GSM (2G) phones that were in use when epidemiological studies that observed a slight increase in the risk for glioma – a malignant type of brain cancer – among heavy users of wireless and cordless telephones were conducted.
Pathophysiology
Brain cancer regions
Meninges
Human brains are surrounded by a system of connective tissue membranes called meninges that separate the brain from the skull. This three-layered covering is composed of (from the outside in) the dura mater (“hard mother”), arachnoid mater (“spidery mother”), and pia mater (“tender mother”). The arachnoid and pia are physically connected and thus often considered as a single layer, the pia-arachnoid, or leptomeninges. Between the arachnoid mater and the pia mater is the subarachnoid space which contains cerebrospinal fluid(CSF). This fluid circulates in the narrow spaces between cells and through the cavities in the brain called ventricles, to nourish, support, and protect the brain tissue. Blood vessels enter the central nervous system through the perivascular space above the pia mater. The cells in the blood vessel walls are joined tightly, forming the blood–brain barrier which protects the brain from toxins that might enter through the blood. Tumours of the meninges are meningiomas and are often benign.
Brain matter
The brains of humans and other vertebrates are composed of very soft tissue and have a gelatin-like texture. Living brain tissue has a pink tint in color on the outside (gray matter), and nearly complete white on the inside (white matter), with subtle variations in color. Three separate brain areas make up most of the brain’s volume:
- telencephalon (cerebral hemispheres or cerebrum)
- mesencephalon (midbrain)
- cerebellum
These areas are composed of two broad classes of cells: neurons and glia. These two types are equally numerous in the brain as a whole, although glial cells outnumber neurons roughly 4 to 1 in the cerebral cortex. Glia come in several types, which perform a number of critical functions, including structural support, metabolic support, insulation, and guidance of development.
Primary tumours of the glial cells are called gliomas and often are malignant by the time they are diagnosed.
Spinal cord and other tissues
The pons is a specific region in the brainstem that consists of myelinated axons much like the spinal cord. The thalamus and hypothalamus of the diencephalon also consist of neuron and glial cell tissue with the hypophysis (pituitary gland) and pineal gland (which is glandular tissue) attached at the bottom; tumours of the pituitary and pineal gland are often benign. The medulla oblongata is at the start of the spinal cord and is composed mainly of neuron tissue enveloped in oligodendrocytes and meninges tissue. The spinal cord is made up of bundles of these axons. Glial cells such as Schwann cells in the periphery or, within the cord itself, oligodendrocytes, wrap themselves around the axon, thus promoting faster transmission of electrical signals and also providing for general maintenance of the environment surrounding the cord, in part by shuttling different compounds around in response to injury or other stimulus.
Diagnosis
A posterior fossa tumour leading to mass effect and midline shift
Although there is no specific or singular symptom or sign, the presence of a combination of symptoms and the lack of corresponding indications of other causes can be an indicator for investigation towards the possibility of an brain tumour. Brain tumours have similar characteristics and obstacles when it comes to diagnosis and therapy with tumours located elsewhere in the body. However, they create specific issues that follow closely to the properties of the organ they are in.
The diagnosis will often start by taking a medical history noting medical antecedents, and current symptoms. Clinical and laboratory investigations will serve to exclude infections as the cause of the symptoms. Examinations in this stage may include the eyes, otolaryngological (or ENT) and electrophysiological exams. The use of electroencephalography (EEG) often plays a role in the diagnosis of brain tumours.
Brain tumours, when compared to tumours in other areas of the body, pose a challenge for diagnosis. Commonly, radioactive tracers are uptaken in large volumes in tumours due to the high activity of tumour cells, allowing for radioactive imaging of the tumour. However, most of the brain is separated from the blood by the blood-brain barrier (BBB), a membrane which exerts a strict control over what substances are allowed to pass into the brain. Therefore, many tracers that may reach tumours in other areas of the body easily would be unable to reach brain tumours until there was a disruption of the BBB by the tumour. Disruption of the BBB is well imaged via MRI or CT scan, and is therefore regarded as the main diagnostic indicator for malignant gliomas, meningiomas, and brain metastases.
Swelling or obstruction of the passage of cerebrospinal fluid (CSF) from the brain may cause (early) signs of increased intracranial pressure which translates clinically into headaches, vomiting, or an altered state of consciousness, and in children changes to the diameter of the skull and bulging of the fontanelles. More complex symptoms such as endocrine dysfunctions should alarm doctors not to exclude brain tumours.
A bilateral temporal visual field defect (due to compression of the optic chiasm) or dilation of the pupil, and the occurrence of either slowly evolving or the sudden onset of focal neurologic symptoms, such as cognitive and behavioral impairment (including impaired judgment, memory loss, lack of recognition, spatial orientation disorders), personality or emotional changes, hemiparesis, hypoesthesia, aphasia, ataxia, visual field impairment, impaired sense of smell, impaired hearing, facial paralysis, double vision, or more severe symptoms such as tremors, paralysis on one side of the body hemiplegia, or (epileptic) seizures in a patient with a negative history for epilepsy, should raise the possibility of a brain tumour.
Imaging
CT scan of a brain tumour, with its diameters marked as an X. There is hypoattenuating (dark) peritumoral edema in the surrounding white matter, with a “finger-like” spread.
Medical imaging plays a central role in the diagnosis of brain tumours. Early imaging methods – invasive and sometimes dangerous – such as pneumoencephalography and cerebral angiography have been abandoned in favor of non-invasive, high-resolution techniques, especially magnetic resonance imaging (MRI) and computed tomography (CT) scans, though MRI is typically the reference standard used. Neoplasms will often show as differently colored masses (also referred to as processes) in CT or MRI results.
- Benign brain tumours often show up as hypodense (darker than brain tissue) mass lesions on CT scans. On MRI, they appear either hypodense or isointense (same intensity as brain tissue) on T1-weighted scans, or hyperintense (brighter than brain tissue) on T2-weighted MRI, although the appearance is variable.
- Contrast agent uptake, sometimes in characteristic patterns, can be demonstrated on either CT or MRI scans in most malignant primary and metastatic brain tumours.
- Pressure areas where the brain tissue has been compressed by a tumour also appear hyperintense on T2-weighted scans and might indicate the presence a diffuse neoplasm due to an unclear outline. Swelling around the tumour known as peritumoral edema can also show a similar result.
This is because these tumours disrupt the normal functioning of the BBB and lead to an increase in its permeability. More recently, advancements have been made to increase the utility of MRI in providing physiological data that can help to inform diagnosis and prognosis. Perfusion Weighted Imaging (PWI) and Diffusion Weighted Imaging (DWI) are two MRI techniques that reviews have been shown to be useful in classifying tumours by grade, which was not previously viable using only structural imaging. However, these techniques cannot alone diagnose high- versus low-grade gliomas, and thus the definitive diagnosis of brain tumour should only be confirmed by histological examination of tumour tissue samples obtained either by means of brain biopsy or open surgery. The histological examination is essential for determining the appropriate treatment and the correct prognosis. This examination, performed by a pathologist, typically has three stages: interoperative examination of fresh tissue, preliminary microscopic examination of prepared tissues, and follow-up examination of prepared tissues after immunohistochemical staining or genetic analysis.
Pathology
Micrograph of an oligodendroglioma, a type of brain cancer. Brain biopsy. H&E stain
Tumours have characteristics that allow determination of malignancy and how they will evolve, and determining these characteristics will allow the medical team to determine the management plan.
Anaplasia or dedifferentiation: loss of differentiation of cells and of their orientation to one another and blood vessels, a characteristic of anaplastic tumour tissue. Anaplastic cells have lost total control of their normal functions and many have deteriorated cell structures. Anaplastic cells often have abnormally high nuclear-to-cytoplasmic ratios, and many are multinucleated. Additionally, the nuclei of anaplastic cells are usually unnaturally shaped or oversized. Cells can become anaplastic in two ways: neoplastic tumour cells can dedifferentiate to become anaplasias (the dedifferentiation causes the cells to lose all of their normal structure/function), or cancer stem cells can increase their capacity to multiply (i.e., uncontrollable growth due to failure of differentiation).
Atypia: an indication of abnormality of a cell (which may be indicative for malignancy). Significance of the abnormality is highly dependent on context.
Neoplasia: the (uncontrolled) division of cells. As such, neoplasia is not problematic but its consequences are: the uncontrolled division of cells means that the mass of a neoplasm increases in size, and in a confined space such as the intracranial cavity this quickly becomes problematic because the mass invades the space of the brain pushing it aside, leading to compression of the brain tissue and increased intracranial pressure and destruction of brain parenchyma. Increased intracranial pressure (ICP) may be attributable to the direct mass effect of the tumour, increased blood volume, or increased cerebrospinal fluid (CSF) volume, which may, in turn, have secondary symptoms.
Necrosis: the (premature) death of cells, caused by external factors such as infection, toxin or trauma. Necrotic cells send the wrong chemical signals which prevent phagocytes from disposing of the dead cells, leading to a buildup of dead tissue, cell debris and toxins at or near the site of the necrotic cells
Arterial and venous hypoxia, or the deprivation of adequate oxygen supply to certain areas of the brain, occurs when a tumour makes use of nearby blood vessels for its supply of blood and the neoplasm enters into competition for nutrients with the surrounding brain tissue.
More generally a neoplasm may cause release of metabolic end products (e.g., free radicals, altered electrolytes, neurotransmitters), and release and recruitment of cellular mediators (e.g., cytokines) that disrupt normal parenchymal function.
Classification
Tumours can be benign or malignant, can occur in different parts of the brain, and may be classified as primary or secondary. A primary tumour is one that has started in the brain, as opposed to a metastatic tumour, which is one that has spread to the brain from another area of the body. The incidence of metastatic tumours is approximately four times greater than primary tumours. Tumours may or may not be symptomatic: some tumours are discovered because the patient has symptoms, others show up incidentally on an imaging scan, or at an autopsy.
Grading of the tumours of the central nervous system commonly occurs on a 4 point scale (I-IV) created by the World Health Organisation in 1993. Grade I tumours are the least severe and commonly associated with long term survival, with severity and prognosis worsening as the grade increases. Low grade tumours are often benign, while higher grades are aggressively malignant and/or metastatic. Other grading scales do exist, many based upon the same criteria as the WHO scale and graded from I-IV.
Primary
The most common primary brain tumours are:
- Gliomas (50.4%)
- Meningiomas (20.8%)
- Pituitary adenomas (15%)
- Nerve sheath tumours (8%)
These common tumours can also be organised according to tissue of origin as shown below:
|
Tissue of origin |
Children | Adults |
|---|---|---|
| Astrocytes | Pilocytic Astrocytoma (PCA) | Glioblastoma Multiforme (GBM) |
| Oligodendrocytes | Oligodendroglioma | |
| Ependyma | Ependymoma | |
| Neurons | Medulloblastoma | |
| Meninges | Meningioma |
Secondary
Secondary tumours of the brain are metastatic and have invaded the brain from cancers originating in other organs. This means that a cancerous neoplasm has developed in another organ elsewhere in the body and that cancer cells have leaked from that primary tumour and then entered the lymphatic system and blood vessels. They then circulate through the bloodstream, and are deposited in the brain. There, these cells continue growing and dividing, becoming another invasive neoplasm of the primary cancer’s tissue. Secondary tumours of the brain are very common in the terminal phases of patients with an incurable metastasized cancer; the most common types of cancers that bring about secondary tumours of the brain are lung cancer, breast cancer, malignant melanoma, kidney cancer, and colon cancer (in decreasing order of frequency).
Secondary brain tumours are more common than primary ones; in the United States there are about 170,000 new cases every year. Secondary brain tumours are the most common cause of tumours in the intracranial cavity. The skull bone structure can also be subject to a neoplasm that by its very nature reduces the volume of the intracranial cavity, and can damage the brain.
By behavior
Brain tumours or intracranial neoplasms can be cancerous (malignant) or non-cancerous (benign). However, the definitions of malignant or benign neoplasms differ from those commonly used in other types of cancerous or non-cancerous neoplasms in the body. In cancers elsewhere in the body, three malignant properties differentiate benign tumours from malignant forms of cancer: benign tumours are self-limited and do not invade or metastasize. Characteristics of malignant tumours include:
- uncontrolled mitosis (growth by division beyond the normal limits)
- anaplasia: the cells in the neoplasm have an obviously different form (in size and shape). Anaplastic cells display marked pleomorphism. The cell nuclei are characteristically extremely hyperchromatic (darkly stained) and enlarged; the nucleus might have the same size as the cytoplasm of the cell (nuclear-cytoplasmic ratio may approach 1:1, instead of the normal 1:4 or 1:6 ratio). Giant cells – considerably larger than their neighbors – may form and possess either one enormous nucleus or several nuclei (syncytia). Anaplastic nuclei are variable and bizarre in size and shape.
- invasion or infiltration (medical literature uses these terms as synonymous equivalents. However, for clarity, the articles that follow adhere to a convention that they mean slightly different things; this convention is not followed outside these articles):
- Invasion or invasiveness is the spatial expansion of the tumour through uncontrolled mitosis, in the sense that the neoplasm invades the space occupied by adjacent tissue, thereby pushing the other tissue aside and eventually compressing the tissue. Often these tumours are associated with clearly outlined tumours in imaging.
- Infiltration is the behavior of the tumour either to grow (microscopic) tentacles that push into the surrounding tissue (often making the outline of the tumour undefined or diffuse) or to have tumour cells “seeded” into the tissue beyond the circumference of the tumorous mass; this does not mean that an infiltrative tumour does not take up space or does not compress the surrounding tissue as it grows, but an infiltrating neoplasm makes it difficult to say where the tumour ends and the healthy tissue starts.
- metastasis (spread to other locations in the body via lymph or blood).
Of the above malignant characteristics, some elements do not apply to primary neoplasms of the brain:
- Primary brain tumours rarely metastasize to other organs; some forms of primary brain tumours can metastasize but will not spread outside the intracranial cavity or the central spinal canal. Due to the BBB, cancerous cells of a primary neoplasm cannot enter the bloodstream and get carried to another location in the body. (Occasional isolated case reports suggest spread of certain brain tumours outside the central nervous system, e.g. bone metastasis of glioblastoma multiforme.)
- Primary brain tumours generally are invasive (i.e. they will expand spatially and intrude into the space occupied by other brain tissue and compress those brain tissues); however, some of the more malignant primary brain tumours will infiltrate the surrounding tissue.
By genetics
In 2016, the WHO restructured their classifications of some categories of gliomas to include distinct genetic mutationsthat have been useful in differentiating tumour types, prognoses, and treatment responses. Genetic mutations are typically detected via immunohistochemistry, a technique that visualises the presence or absence of a targeted protein via staining.
- Mutations in IDH1 and IDH2 genes are commonly found in low grade gliomas
- Loss of both IDH genes combined with loss of chromosome arms 1p and 19q indicates the tumour is an oligodendroglioma
- Loss of TP53 and ATRX characterises astrocytomas
- Genes EFGR, TERT, and PTEN, are commonly altered in gliomas and are useful in differentiating tumour grade and biology
Specific types
Anaplastic astrocytoma, Astrocytoma, Central neurocytoma, Choroid plexus carcinoma, Choroid plexus papilloma, Choroid plexus tumour, Dysembryoplastic neuroepithelial tumour, Ependymal tumour, Fibrillary astrocytoma, Giant-cell glioblastoma, Glioblastoma multiforme, Gliomatosis cerebri, Gliosarcoma, Hemangiopericytoma, Medulloblastoma, Medulloepithelioma, Meningeal carcinomatosis, Neuroblastoma, Neurocytoma, Oligoastrocytoma, Oligodendroglioma, Optic nerve sheath meningioma, Pediatric ependymoma, Pilocytic astrocytoma, Pinealoblastoma, Pineocytoma, Pleomorphic anaplastic neuroblastoma, Pleomorphic xanthoastrocytoma, Primary central nervous system lymphoma, Sphenoid wing meningioma, Subependymal giant cell astrocytoma, Subependymoma, Trilateral retinoblastoma.
Treatment
A medical team generally assesses the treatment options and presents them to the person affected and their family. Various types of treatment are available depending on tumour type and location, and may be combined to produce the best chances of survival:
- Surgery: complete or partial resection of the tumour with the objective of removing as many tumour cells as possible.
- Radiotherapy: the most commonly used treatment for brain tumours; the tumour is irradiated with beta, x rays or gamma rays.
- Chemotherapy: a treatment option for cancer, however, it is not always used to treat brain tumours as the blood-brain barrier can prevent some drugs from reaching the cancerous cells.
- A variety of experimental therapies are available through clinical trials.
Survival rates in primary brain tumours depend on the type of tumour, age, functional status of the patient, the extent of surgical removal and other factors specific to each case.
Surgery
The primary and most desired course of action described in medical literature is surgical removal (resection) via craniotomy. Minimally invasive techniques are becoming the dominant trend in neurosurgical oncology. The main objective of surgery is to remove as many tumour cells as possible, with complete removal being the best outcome and cytoreduction (“debulking”) of the tumour otherwise. In some cases access to the tumour is impossible and impedes or prohibits surgery.
Many meningiomas, with the exception of some tumours located at the skull base, can be successfully removed surgically. Most pituitary adenomas can be removed surgically, often using a minimally invasive approach through the nasal cavity and skull base (trans-nasal, trans-sphenoidal approach). Large pituitary adenomas require a craniotomy (opening of the skull) for their removal. Radiotherapy, including stereotactic approaches, is reserved for inoperable cases.
Several current research studies aim to improve the surgical removal of brain tumours by labeling tumour cells with 5-aminolevulinic acid that causes them to fluoresce. Postoperative radiotherapy and chemotherapy are integral parts of the therapeutic standard for malignant tumours. Radiotherapy may also be administered in cases of “low-grade” gliomas when a significant tumour reduction could not be achieved surgically.
Multiple metastatic tumours are generally treated with radiotherapy and chemotherapy rather than surgery and the prognosis in such cases is determined by the primary tumour, and is generally poor.
Radiation therapy
The goal of radiation therapy is to kill tumour cells while leaving normal brain tissue unharmed. In standard external beam radiation therapy, multiple treatments of standard-dose “fractions” of radiation are applied to the brain. This process is repeated for a total of 10 to 30 treatments, depending on the type of tumour. This additional treatment provides some patients with improved outcomes and longer survival rates.
Radiosurgery is a treatment method that uses computerised calculations to focus radiation at the site of the tumour while minimising the radiation dose to the surrounding brain. Radiosurgery may be an adjunct to other treatments, or it may represent the primary treatment technique for some tumours. Forms used include stereotactic radiosurgery, such as Gamma knife, Cyberknife or Novalis Tx radiosurgery.
Radiotherapy is the most common treatment for secondary brain tumours. The amount of radiotherapy depends on the size of the area of the brain affected by cancer. Conventional external beam “whole-brain radiotherapy treatment” (WBRT) or “whole-brain irradiation” may be suggested if there is a risk that other secondary tumours will develop in the future. Stereotactic radiotherapy is usually recommended in cases involving fewer than three small secondary brain tumours. Radiotherapy may be used following, or in some cases in place of, resection of the tumour. Forms of radiotherapy used for brain cancer include external beam radiation therapy, the most common, and brachytherapy and proton therapy, the last especially used for children.
People who receive stereotactic radiosurgery (SRS) and whole-brain radiation therapy (WBRT) for the treatment of metastatic brain tumours have more than twice the risk of developing learning and memory problems than those treated with SRS alone.
Chemotherapy
Patients undergoing chemotherapy are administered drugs designed to kill tumour cells. Although chemotherapy may improve overall survival in patients with the most malignant primary brain tumours, it does so in only about 20 percent of patients. Chemotherapy is often used in young children instead of radiation, as radiation may have negative effects on the developing brain. The decision to prescribe this treatment is based on a patient’s overall health, type of tumour, and extent of the cancer. The toxicity and many side effects of the drugs, and the uncertain outcome of chemotherapy in brain tumours puts this treatment further down the line of treatment options with surgery and radiation therapy preferred.
UCLA Neuro-Oncology publishes real-time survival data for patients with a diagnosis of glioblastoma multiforme. They are the only institution in the United States that displays how brain tumour patients are performing on current therapies. They also show a listing of chemotherapy agents used to treat high-grade glioma tumours.
Genetic mutations have significant effects on the effectiveness of chemotherapy. Gliomas with IDH1 or IDH2 mutations respond better to chemotherapy than those without the mutation. Loss of chromosome arms 1p and 19q also indicate better response to chemoradiation.
Other
A shunt may be used to relieve symptoms caused by intracranial pressure, by reducing the build-up of fluid (hydrocephalus) caused by the blockage of the free flow of cerebrospinal fluid.
Prognosis
The prognosis of brain cancer depends on the type of cancer diagnosed. Medulloblastoma has a good prognosis with chemotherapy, radiotherapy, and surgical resection while glioblastoma multiforme has a median survival of only 12 months even with aggressive chemoradiotherapy and surgery. Brainstem gliomas have the poorest prognosis of any form of brain cancer, with most patients dying within one year, even with therapy that typically consists of radiation to the tumour along with corticosteroids. However, one type, focal brainstem gliomas in children, seems open to exceptional prognosis and long-term survival has frequently been reported.
Prognosis is also affected by presentation of genetic mutations. Certain mutations provide better prognosis than others. IDH1 and IDH2 mutations in gliomas, as well as deletion of chromosome arms 1p and 19q, generally indicate better prognosis. TP53, ATRX, EGFR, PTEN, and TERT mutations are also useful in determining prognosis.
Glioblastoma multiforme
Glioblastoma multiforme (GBM) is the most aggressive (grade IV) and most common form of a malignant brain tumour. Even when aggressive multimodality therapy consisting of radiotherapy, chemotherapy, and surgical excision is used, median survival is only 12–17 months. Standard therapy for glioblastoma multiforme consists of maximal surgical resection of the tumour, followed by radiotherapy between two and four weeks after the surgical procedure to remove the cancer, then by chemotherapy, such as temozolomide. Most patients with glioblastoma take a corticosteroid, typically dexamethasone, during their illness to relieve symptoms. Experimental treatments include targeted therapy, gamma knife radiosurgery, boron neutron capture therapy and gene therapy.
Oligodendrogliomas
Oligodendrogliomas are incurable but slowly progressive malignant brain tumours. They can be treated with surgical resection, chemotherapy, radiotherapy or a combination. For some suspected low-grade (grade II) tumours, only a course of watchful waiting and symptomatic therapy is opted for. These tumours show a high frequency of co-deletions of the p and q arms of chromosome 1 and chromosome 19 respectively (1p19q co-deletion) and have been found to be especially chemosensitive with one report claiming them to be one of the most chemosensitive tumours. A median survival of up to 16.7 years has been reported for grade II oligodendrogliomas.
Epidemiology
Figures for incidences of cancers of the brain show a significant difference between more- and less-developed countries (the less-developed countries have lower incidences of tumours of the brain). This could be explained by undiagnosed tumour-related deaths (patients in extremely poor situations do not get diagnosed, simply because they do not have access to the modern diagnostic facilities required to diagnose a brain tumour) and by deaths caused by other poverty-related causes that preempt a patient’s life before tumours develop or tumours become life-threatening. Nevertheless, statistics suggest that certain forms of primary brain tumours are more common among certain populations.
The incidence of low-grade astrocytoma has not been shown to vary significantly with nationality. However, studies examining the incidence of malignant central nervous system (CNS) tumours have shown some variation with national origin. Since some high-grade lesions arise from low-grade tumours, these trends are worth mentioning. Specifically, the incidence of CNS tumours in the United States, Israel, and the Nordic countries is relatively high, while Japan and Asian countries have a lower incidence. These differences probably reflect some biological differences as well as differences in pathologic diagnosis and reporting. Worldwide data on incidence of cancer can be found at the WHO (World Health Organisation) and is handled by the IARC (International Agency for Research on Cancer) located in France.
United States
In the United States in 2015, approximately 166,039 people were living with brain or other central nervous system tumours. Over 2018, it was projected that there would be 23,880 new cases of brain tumours and 16,830 deaths in 2018 as a result, accounting for 1.4 percent of all cancers and 2.8 percent of all cancer deaths. Median age of diagnosis was 58 years old, while median age of death was 65. Diagnosis was slightly more common in males, at approximately 7.5 cases per 100 000 people, while females saw 2 fewer at 5.4. Deaths as a result of brain cancer were 5.3 per 100 000 for males, and 3.6 per 100 000 for females, making brain cancer the 10th leading cause of cancer death in the United States. Overall lifetime risk of developing brain cancer is approximated at 0.6 percent for men and women.
UK
Brain, other CNS or intracranial tumours are the ninth most common cancer in the UK (around 10,600 people were diagnosed in 2013), and it is the eighth most common cause of cancer death (around 5,200 people died in 2012).
Children
In the United States more than 28,000 people under 20 are estimated to have a brain tumour. About 3,720 new cases of brain tumours are expected to be diagnosed in those under 15 in 2019. Higher rates were reported in 1985–1994 than in 1975–1983. There is some debate as to the reasons; one theory is that the trend is the result of improved diagnosis and reporting, since the jump occurred at the same time that MRIs became available widely, and there was no coincident jump in mortality. They are 20–25 percent of cancers in children.
The average survival rate for all primary brain cancers in children is 74%. Brain cancers are the most common cancer in children under 19, are result in more death in this group than leukemia. Younger people do less well.
The most common brain tumour types in children (0-14) are: pilocytic astrocytoma, malignant glioma, medulloblastoma, neuronal and mixed neuronal-glial tumours, and ependymoma.
In children under 2, about 70% of brain tumours are medulloblastomas, ependymomas, and low-grade gliomas. Less commonly, and seen usually in infants, are teratomas and atypical teratoid rhabdoid tumours. Germ cell tumours, including teratomas, make up just 3% of pediatric primary brain tumours, but the worldwide incidence varies significantly.
In the UK, 429 children aged 14 and under are diagnosed with a brain tumour on average each year, and 563 children and young people under the age of 19 are diagnosed.
Research
Immunotherapy
Cancer immunotherapy is being actively studied. For malignant gliomas no therapy has been shown to improve life expectancy as of 2015.
Vesicular stomatitis virus
In 2000, researchers used the vesicular stomatitis virus, or VSV, to infect and kill cancer cells without affecting healthy cells.
A brainstem glioma in four-year-old. MRI, sagittal, without contrast
Led by Prof. Nori Kasahara, researchers from USC, who are now at UCLA, reported in 2001 the first successful example of applying the use of retroviral replicating vectors towards transducing cell lines derived from solid tumours. Building on this initial work, the researchers applied the technology to in vivomodels of cancer and in 2005 reported a long-term survival benefit in an experimental brain tumour animal model. Subsequently, in preparation for human clinical trials, this technology was further developed by Tocagen (a pharmaceutical company primarily focused on brain cancer treatments) as a combination treatment (Toca 511 & Toca FC). This has been under investigation since 2010 in a Phase I/II clinical trial for the potential treatment of recurrent high-grade glioma including glioblastoma multiforme (GBM) and anaplastic astrocytoma. No results have yet been published.
Year Observances
June Observances
Join us on Telegram Channel: @worldcelebrationdays (It is not a group)
Web Telegram in Browser : https://web.telegram.org/k/#@worldcelebrationdays
Twitter:
Hashtags:
#WorldBrainTumourDay #braintumourday #brain #Tumour #event #JUNE #WorldDay #InternationalDay #NationalDay #CelebrationDay #HappyDay #Celebration #Observances #Programme #information #TelegramTips #whatsappdown #DeleteWhatsApp #JUN #telegramchannel #World #International #Nation .
Join us on Twitter Follow: @worldinformativ
https://twitter.com/worldinformativ
LinkedIn:
Hashtags:
#worldbraintumourday #braintumourday #brain #tumour #event #june #worldday #internationalday #nationalday #celebrationday #happyday #programmes #informations #observances #telegramtips #twitter #linkedinnewsletter #telegramchannel #whatsappdown #deletewhatsapp #Jun . #world #internationalisation #celebrationdays #celebrations #events .
Click here: https://lnkd.in/dVTdD6E4
Join us on LinkedIn Follow:
https://www.linkedin.com/company/informativeandentertaining/
Microsoft Teams:

Microsoft Teams Channel : https://teams.live.com/l/community/FEA-Z68SQNIePDj_gg
Telegram:
Hashtags:
#WorldBrainTumourDay #BrainTumourDay #Brain #Tumour #Event #June #WorldDay #InternationalDay #NationalDay #CelebrationDay #HappyDay #Programme #Information #Observances #TelegramTips @Telegram #TelegramChannel #Twitter #LinkedinNewsletter #WhatsAppDown #DeleteWhatsApp #Jun . #World #International #Nation #CelebrationDays #Celebration #Happy #Events .
Join us on Telegram Channel: @worldcelebrationdays
Web Telegram in Browser : https://web.telegram.org/k/#@worldcelebrationdays
https://t.me/worldcelebrationdays
Facebook:
Hashtags:
#WorldBrainTumourDay #braintumourday #Brain #tumour #event #June #WorldDay #InternationalDay #NationalDay #CelebrationDay #HappyDay #Observances #Programme #information #TelegramTips #TelegramChannel #LinkedinNewsletter #Celebration #Jun . #National #world #international #CelebrationDays #celebrations #happy #Events .
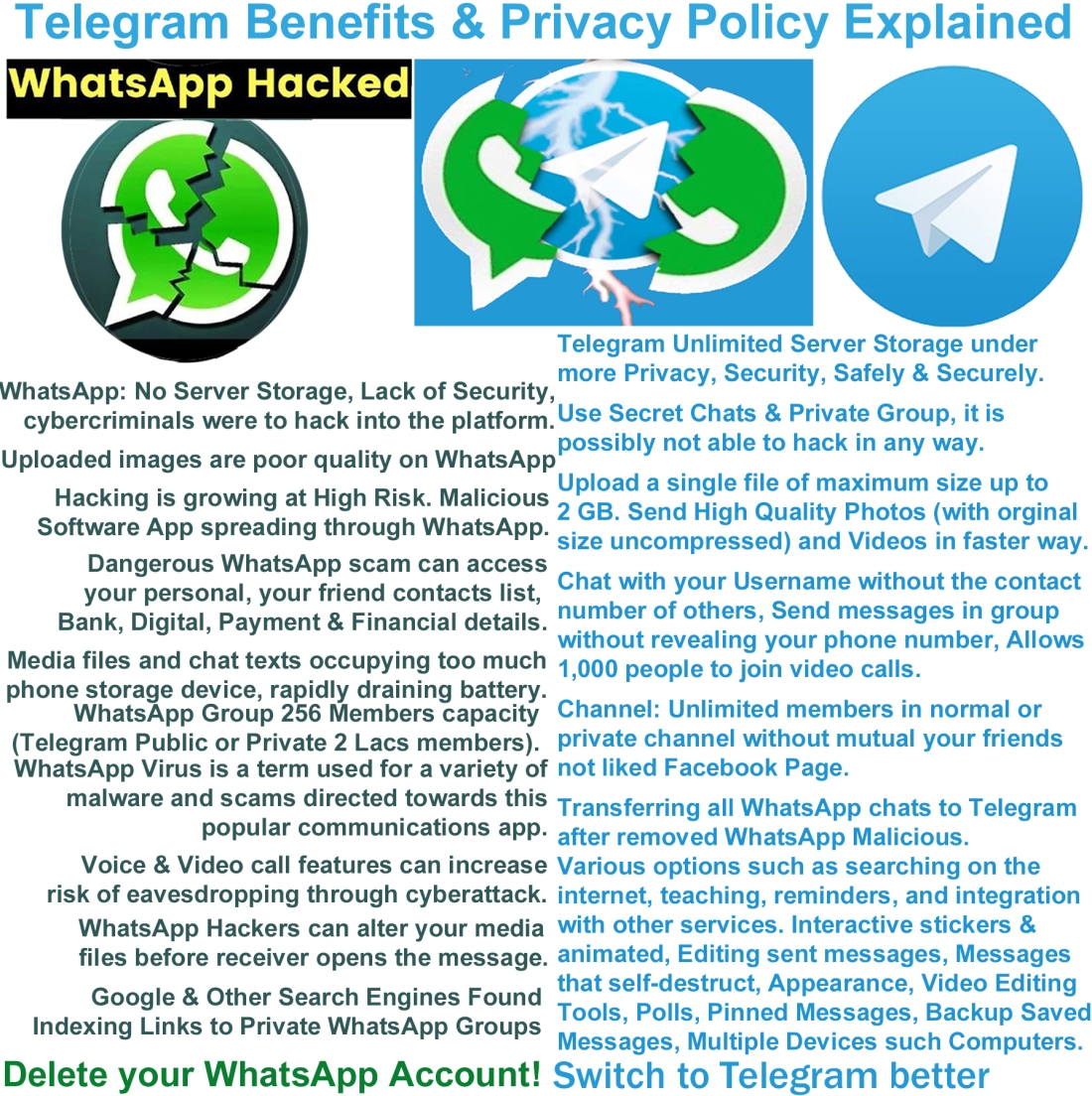
Better Way: Delete your WhatsApp and Change to Telegram
WhatsApp : Illegal Effect : Hacking is growing at High Risk in future
(1) WhatsApp does not store messages on its servers, so if cybercriminals were to hack into the platform, they would not be able to decrypt any of the messages.
Telegram is a cloud service. We store messages, photos, videos and documents from your cloud chats on our servers so that you can access your data from any of your devices anytime without having to rely on third-party backups. This way local engineers or physical intruders cannot get access to user data.
(2) (a) Additionally, WhatsApp does not have the key to see encrypted messages. By default, WhatsApp stores messages in a way that allows them to be backed up to the cloud by iOS or Android. WhatsApp store in phone storage device occupies more space.
(2) (b) WhatsApp files (photos, audios, videos, documents) and texts occupying too much phone storage device. Read more…Click here to open link.
https://www.businesstoday.in/technology/news/story/whatsapp-files-occupying-too-much-phone-storage-heres-what-you-can-do-279321-2020-11-21 to view webpage with the browser.
Telegram provides unlimited cloud storage. This means all your text messages, images media files & documents will be saved on their cloud without losing any data, you don’t need to worry about backup & restore.
(3) WhatsApp: Uncrackable problem of end-to-end encryption: Lack of Security
Telegram Secret Chats are one-on-one chats wherein messages are encrypted with a key held only by the chat’s participants. Note that the schema for these end-to-end encrypted Secret Chats is different from what is used for cloud chats.
(4) WhatsApp Draining Your Phone’s Battery Too? This Could Be The Reason. Read more…Click here to open link.
https://www.republicworld.com/technology-news/apps/whatsapp-draining-your-phones-battery-too-this-could-be-the-reason.html to view webpage with the browser.
(5) WhatsApp warning: How a single phone call hacked phones worldwide. Read more…Click here to open link.
https://www.express.co.uk/life-style/science-technology/1276195/WhatsApp-hack-how-single-call-compromised-phones to view webpage with the browser.
(6) WhatsApp virus is a term used for a variety of malware and scams directed towards this popular communications app. Read more…Click here to open link.
https://www.2-spyware.com/remove-whatsapp-virus.html#qm-h2-1 to view webpage with the browser.
(7) New Warning for WhatsApp Users Over Account Suspension ‘Hack’. Read more…Click here to open link.
https://www.forbes.com/sites/zakdoffman/2021/04/10/shock-new-warning-for-millions-of-whatsapp-users-on-apple-iphone-and-google-android-phones/?sh=2b33ce0d7585 to view webpage with the browser.
Telegram Privacy Policy: Read more: https://telegram.org/privacy
(8) This dangerous WhatsApp scam can access your personal and financial details. Read more…Click here to open link.
https://www.gadgetsnow.com/tech-news/this-dangerous-whatsapp-scam-can-access-your-personal-and-financial-details/articleshow/88519735.cms to view webpage with the browser.
(9) Your WhatsApp, Facebook data isn’t safe! Malicious apps that steal data found on Play Store. Read more…Click here to open link.
https://www.businesstoday.in/buzztop/buzztop-technology/your-whatsapp-facebook-data-isnt-safe-malicious-apps-that-steal-data-found-on-play-store/story/307472.html to view webpage with the browser.
(10) Dangerous new spyware can steal your WhatsApp messages and take photos using your smartphone camera without your permission and admit it’s been around for FIVE YEARS already. Read more…Click here to open link.
https://www.thesun.co.uk/tech/5359250/what-is-skygofree-spyware-how-to-stay-safe-whatsapp/ to view webpage with the browser.
(11) One of the most-advanced Android malware discovered; can even ‘steal’ your WhatsApp messages. Read more…Click here to open link.
https://cio.economictimes.indiatimes.com/news/digital-security/one-of-the-most-advanced-android-malware-discovered-can-even-steal-your-whatsapp-messages/62548876 to view webpage with the browser.
(12) One billion users of the messaging service are now promised full encryption. Which can only mean the spooks will retaliate elsewhere. Read more…Click here to open link.
https://www.theguardian.com/commentisfree/2016/apr/10/whatsapp-encryption-billion-users-data-security to view webpage with the browser.
(13) Wormable Android malware is spreading through WhatsApp messages. Read more…Click here to open link.
https://www.itpro.co.uk/security/malware/359133/new-android-malware-discovered-that-spreads-through-whatsapp-messages to view webpage with the browser.
(14) Malicious WhatsApp mod infects Android devices with malware. Read more…Click here to open link.
https://www.bleepingcomputer.com/news/security/malicious-whatsapp-mod-infects-android-devices-with-malware/ to view webpage with the browser.
(15) WhatsApp joinable calls feature can increase risk of eavesdropping through cyberattack: Kaspersky. Read more…Click here to open link.
https://telecom.economictimes.indiatimes.com/news/whatsapp-joinable-calls-feature-can-increase-risk-of-eavesdropping-through-cyberattack-kaspersky/84640328 to view webpage with the browser.
(16) WhatsApp hijack scam continues to spread. Read more…Click here to open link.
https://www.bbc.com/news/technology-57357301.amp to view webpage with the browser.
(17) 8 Ways Your WhatsApp Messages Can Be Hacked. Read more…Click here to open link.
https://www.makeuseof.com/tag/how-whatsapp-messages-can-hacked/ to view webpage with the browser.
Telegram Messenger Web ( https://web.telegram.org/#/login ) always easy and faster than all emails (Gmail, Hotmail, Outlook, Microsoft Office 365, Yahoo mail, AOL, etc) and also Instant Messenger. Available on the Telegram Desktop for Microsoft Windows / Apple Mac / Linux. Telegram Messenger is better than WhatsApp, Signal, WhatsApp Business, Microsoft Kaizala, WeChat, Hike, Line, Viber, Hangouts, BBM & Facebook Messenger for saving battery and phone storage with your Smartphone. Telegram for iPhone / iPad available on the App Store for iOS devices. https://telegram.org

NOTE: Microsoft Kaizala has retired on 31st August 2023. Kaizala moved to Microsoft Teams from 1st September 2023.
NOTE: Microsoft Kaizala has retired on 31st August 2023. Kaizala moved to Microsoft Teams from 1st September 2023.
NOTE: Microsoft Kaizala has retired on 31st August 2023. Kaizala moved to Microsoft Teams from 1st September 2023.
Telegram provides unlimited cloud storage. This means all your text messages, images media files & documents will be saved on their cloud without losing any data, you don’t need to worry about backup & restore. Telegram Private Groups cannot be found with an in-app search. The group is private, after all that you can use the 2,00,000 member limit fully. Telegram Channels are a tool for broadcasting public (or) private messages to large audiences, similarly as you do on Twitter or Facebook Page. In fact, channels can have an unlimited number of subscribers. Telegram Private Channels cannot be found with an in-app search. Group video calls on Telegram allow 30 users to broadcast from their camera as well as their screens. This can now be watched by 1,000 people at once (updated by 1st August 2021). Users can hold anything event online, from lectures to concerts and everything in between, similarly as Zoom or Microsoft Teams or Google Meet.
A. Simple: Telegram is so simple you already know how to use it.
B. Private: Telegram messages are heavily encrypted and can self-destruct.
C. Synced: Telegram lets you access your chats from multiple devices.
D. Fast: Telegram delivers messages faster than any other application such WhatsApp, Signal etc.
E. Powerful: Telegram has no limits on the size of your media and chats.
F. Open: Telegram has an open API and source code free for everyone.
G. Secure: Telegram keeps your messages safe from hacker attacks.
H. Expressive: Telegram lets you completely customise your messenger.
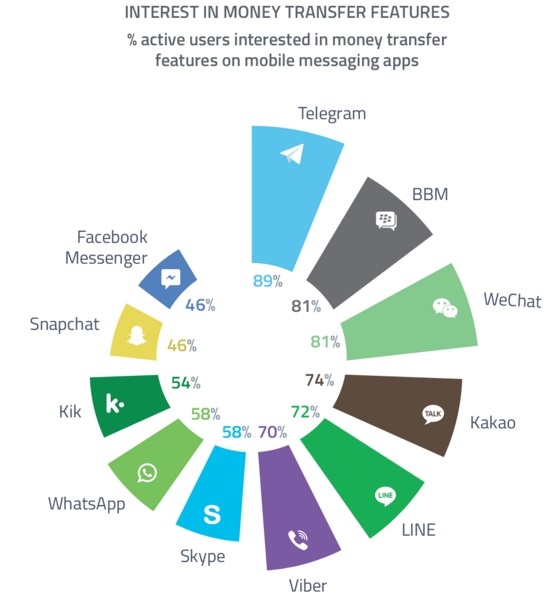
Telegram: Interest in Money Transfer Features % active users on BBM, WeChat, Kakao, LINE, Viber, Skype, WhatsApp, Kik, Snapchat and Facebook Messenger.
World Informative & Entertaining:
[ https://worldinformative.wordpress.com/ ]
![]()
Web Telegram in Browser : https://web.telegram.org/k/#@worldcelebrationdays
World Celebration Days
| Telegram Channel | Twitter | LinkedIn Page | Microsoft Teams | Other Social | WhatsApp Channel | Blogger |
All Guests Viewed since 2010: Counter: